PROSTATE HEALTH
Benign Prostatic Hyperplasia (BPH)
Previously we discussed the location and functionality of the organ called the prostate and some symptoms that indicate a prostate problem.
Can you imagine being pressed but unable to release the urine out of your system, no matter how hard you tried?
The discomfort, lower abdominal swelling, and pain are better imagined than experienced. Those who have experienced it once would not wish it upon their worst enemy.
What is BPH?
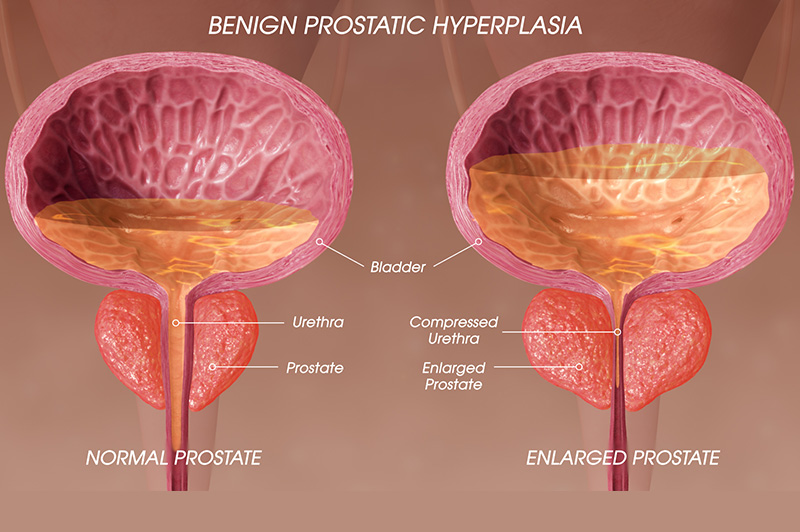
Benign Prostatic Hyperplasia (BPH) is an enlargement of the prostate which often begins from the age of 50 years. The enlarging prostate presses down on the urethra, resulting in a variety of problems with passing urine.
What causes an enlarged prostate?
The prostate enlargement is attributable to different factors such as an increase in age, and levels of certain hormones including that produced by the testes -testosterone. Eunuchs (castrated men) do not develop BPH, hence the evidence that lack of testosterone production can prevent BPH.
Urinary retention (inability to pass urine despite a full bladder) is one of the most distressing symptoms of an enlarged prostate, often causing an individual to rush into the emergency department in excruciating pain.
Who is at risk of prostate enlargement?
All males over age 50 are at risk of having prostate enlargement. The risk is also higher in those who are obese, have a family member who had BPH, and have high blood pressure, high blood sugar, and cholesterol levels.
Though all men are at risk, African men have a higher chance of a faster increase in size and worse symptoms because they generally have a higher level of testosterone and other hormones that cause the problem.
What are the things that show the prostate might be enlarged?
Symptoms of BPH may be mild, meaning that it causes little or no distress to the individual. Mild symptoms may not cause much distress. Moderate to severe symptoms, however, are more discomforting with the need to commence treatment immediately to avoid complications. Most of the symptoms are disturbances in the way a person passes urine, viz:
- Urinating too frequently (frequency). This happens because the pressure on the urethra goes back to the storage tank (bladder). The urinary bladder becomes more sensitive, for it then contracts to remove any little urine that comes in.
- Inability to hold in urine until a more convenient time (Urgency).
- A time lag between the straining and release of urine (hesitancy).
- The urine comes out gradually, sometimes in drops (poor urine stream).
- Pushing hard before urine starts coming out (straining).
- Feeling that there’s still urine that is yet to come out after easing yourself.
- Having some urine drop out a while after using the loo without an urge to urinate (dribbling).
How is BPH diagnosed?
Your doctor will ask you about your symptoms and then examine your body. This will involve putting a lubricated finger into your anus to access your prostate. This examination is quite uncomfortable but not painful per se, as the examination finger is well lubricated.
Then your doctor may request some blood tests, urine tests, and scans to confirm the diagnosis and to check for complications, before drawing up a treatment plan. You may be referred to a urologist (a surgeon that treats problems of the urinary and genital tracts) if you were first seen by a physician.
Treatment
The treatment of BPH begins with lifestyle changes and then medications. As the disease progresses, surgical procedures may then be needed as a definitive treatment to relieve symptoms permanently.
Lifestyle changes that help to reduce symptoms and progression are:
- Abstinence from alcohol and caffeine-containing drinks such as coffee, cola, and energy drinks. These increase the need to pee often and bladder irritation.
- Avoidance of excessive fluid intake at bedtime to reduce the need to wake up at night to urinate.
- Exercising regularly. It helps to control the risk factors of BPH such as obesity.
- Avoidance of drugs for catarrh or common cold (nasal decongestant and antihistamines) and some pain medications such as diclofenac. This is because they may reduce bladder contraction and cause incomplete emptying, or in extreme cases, acute urinary retention.
- Avoid postponing urinating when you have the urge and wait a moment after urinating to try again.
Drug treatment is with tablets that help reduce the production of hormones that cause prostate enlargement or the effect of the hormones on the prostate.
Surgical treatment is to remove the prostate either through the opening at the tip of the penis (urethra) or through the abdomen.
Is there any after effect of the removal of the prostate?
Many people fear that sexual activity may not remain the same after surgical removal of the prostate. This is not too far from the truth in the first few months after surgery.
There is the risk of difficulty achieving an erection (erectile dysfunction), ejaculating, and difficulty controlling urine which is highest in the immediate future after surgery.
However, these are not life-threatening conditions when compared with complications that may arise if BPH is not definitively treated. In addition, they can be managed and resolved eventually in most cases.
The complications that may arise from not treating BPH include kidney stones, recurrent urinary tract infections, kidney failure, etc.
When I worked in the urology unit several years ago, many elderly male patients diagnosed with BPH were having indwelling urethral catheters (a plastic pipe passed into the bladder through the penis and connected to a urine bag) being changed every 3 to 4 weeks. Some were so afraid of surgery and the complications, that they preferred these frequent catheter changes.
Nowadays, there are newer surgical procedures that have fewer complications and preserve sexual function afterward.
Do not let the fear of the inability to get an erection deny you a life-saving procedure that can improve your quality of life. Why keep changing catheters, go through the pain of urinary retention, recurrent infections, or stand the risk of kidney stones and kidney failure?
We will explain the complications that may arise from lack of or delayed treatment of BPH in the next post.
Do you want to know the foods you can eat to prevent or at least slow the progression of BPH? Look out for the next post.